
What is depression ?
Depression is a mental health condition that affects millions of people worldwide. It’s not just feeling sad or down, but rather a persistent and overwhelming sense of hopelessness, worthlessness, and emotional pain that can make even simple tasks seem impossible. Symptoms of depression can vary from person to person but commonly include low energy, changes in appetite or sleep patterns, difficulty concentrating, and losing interest in activities once enjoyed. While it’s normal for everyone to feel sad at times, depression differs in its duration and intensity.
Symptoms of depression
Depression can manifest in various ways, and symptoms can vary from person to person. However, common signs and symptoms of depression include:
- Persistent sadness or low mood: Feeling down, hopeless, or empty most of the time.
- Loss of interest or pleasure in activities: Losing interest in activities once enjoyed, such as hobbies, socializing, or sex.
- Changes in appetite or weight: Significant weight loss or gain due to changes in appetite.
- Sleep disturbances: Difficulty falling asleep, staying asleep, or oversleeping.
- Fatigue or low energy: Feeling tired and lacking energy, even after rest.
- Feelings of worthlessness or guilt: Feeling worthless, helpless, or excessively guilty about past actions.
- Difficulty concentrating or making decisions: Trouble focusing, remembering details, or making decisions.
It’s important to note that experiencing some of these symptoms occasionally does not necessarily mean someone has depression. However, if these symptoms persist for two weeks or longer and interfere with daily functioning and quality of life, it’s essential to seek professional help. Depression is a treatable condition, and early intervention can make a significant difference in recovery.
Classification of depression
Depression can be classified into various types based on factors such as duration, severity, and underlying causes. Some common classifications of depression include:
- Major Depressive Disorder (MDD)
- Persistent Depressive Disorder (PDD)
- Bipolar Disorder
- Seasonal Affective Disorder (SAD)
- Psychotic Depression
- Postpartum Depression (PPD)
These are just a few examples of how depression can be classified. Each type of depression may have its own specific symptoms, risk factors, and treatment approaches. It’s essential for individuals experiencing symptoms of depression to seek evaluation and treatment from a qualified healthcare professional.
Cause of depression
Depression is a complex condition with multiple potential causes, and it often results from a combination of genetic, biological, environmental, and psychological factors.
Some common causes and risk factors for depression include:
- Genetics: A family history of depression or other mood disorders can increase the risk of developing depression. While specific genes associated with depression have been identified, genetics alone do not determine whether someone will develop depression.
- Brain chemistry and biology: Imbalances in certain neurotransmitters (such as serotonin, dopamine, and norepinephrine) and changes in brain structure and function can contribute to depression. These biological factors can affect mood regulation, emotional processing, and stress response.
- Psychological factors: Certain personality traits, coping styles, and thought patterns can increase the risk of depression. For example, individuals with low self-esteem, perfectionistic tendencies, or a history of trauma or abuse may be more susceptible to depression.
- Environmental factors: Stressful life events, such as loss, trauma, financial difficulties, relationship problems, or chronic illness, can trigger or exacerbate depression. Additionally, ongoing stress from work, school, or caregiving responsibilities can contribute to the development of depression.
- Medical conditions: Chronic medical conditions such as diabetes, cardiovascular disease, cancer, and neurological disorders can increase the risk of depression. Some medications used to treat these conditions may also have depression as a side effect.
- Substance abuse: Substance abuse and addiction can co-occur with depression, as individuals may use drugs or alcohol as a way to cope with negative emotions. Substance abuse can worsen depression symptoms and interfere with treatment effectiveness.
- Hormonal changes: Fluctuations in hormone levels, such as those that occur during puberty, pregnancy, childbirth, menopause, or thyroid disorders, can contribute to mood disturbances and increase the risk of depression.
It’s important to recognize that depression is a complex and multifaceted condition, and not everyone with risk factors will develop depression, nor will those without risk factors be immune to it. Seeking professional help from a healthcare provider or mental health professional is essential for accurate diagnosis and effective treatment tailored to individual needs.
Some effective treatment options for depression
Certainly! Effective treatment options for depression include:
- Therapy/Counseling: Psychotherapy, such as cognitive-behavioral therapy (CBT), interpersonal therapy (IPT), or psychodynamic therapy, can help individuals explore and address underlying issues contributing to depression. Therapy provides a supportive space to learn coping skills, challenge negative thought patterns, and develop healthier ways of thinking and behaving.
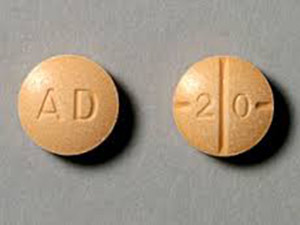
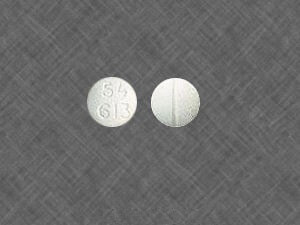
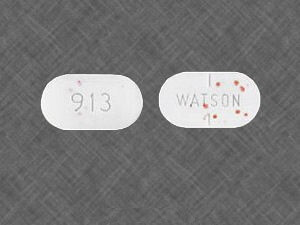
- Medication: Antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), or atypical antidepressants, may be prescribed by a healthcare provider to help alleviate symptoms of depression by balancing neurotransmitter levels in the brain.
- Combination Therapy: For moderate to severe depression, a combination of therapy and medication may be recommended to achieve optimal symptom relief. This approach addresses both the psychological and biological aspects of depression.
- Electroconvulsive Therapy (ECT): ECT is a medical procedure in which electrical currents are passed through the brain to induce a controlled seizure, effectively altering brain chemistry and relieving symptoms of severe depression. ECT is typically considered when other treatments have not been effective or when rapid relief is needed.
- Transcranial Magnetic Stimulation (TMS): TMS is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain, particularly in areas implicated in depression. TMS is often used as an alternative treatment for individuals who have not responded to antidepressant medication.
- Light Therapy: Light therapy, or phototherapy, involves exposure to bright artificial light, typically used to treat seasonal affective disorder (SAD) and certain types of depression with a seasonal pattern. Light therapy helps regulate circadian rhythms and improve mood by increasing serotonin levels in the brain.
- Exercise: Regular physical activity, such as aerobic exercise, strength training, or yoga, has been shown to have mood-boosting effects and reduce symptoms of depression by increasing the production of endorphins and promoting neuroplasticity.
- Nutritional Support: Consuming a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can support overall mental and physical well-being. Some studies suggest that certain nutrients, such as omega-3 fatty acids and folate, may have specific benefits for mood regulation.
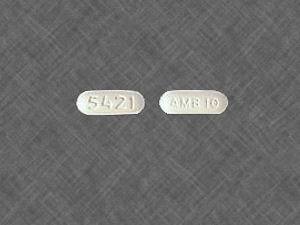
- Sleep Hygiene: Establishing a consistent sleep schedule, creating a relaxing bedtime routine, and practicing good sleep hygiene habits can improve sleep quality and help regulate mood.
- Mindfulness and Meditation: Mindfulness practices, such as meditation, deep breathing exercises, and body scans, can cultivate present-moment awareness and promote relaxation, reducing symptoms of depression.
It’s important for individuals with depression to work closely with healthcare professionals to determine the most appropriate treatment plan based on their specific needs, preferences, and severity of symptoms. Combination approaches, lifestyle modifications, and ongoing support can contribute to long-term recovery and well-being.
Lifestyle Interventions for Managing Depression
Depression, a complex and multifaceted mental health condition, affects millions of people worldwide. While traditional treatments such as therapy and medication play crucial roles in managing depression, lifestyle interventions offer additional avenues for support and symptom relief. Lifestyle interventions encompass various behaviors and habits that individuals can adopt to promote mental well-being and alleviate depressive symptoms. In this essay, we will explore the importance of lifestyle interventions in managing depression and discuss specific strategies that individuals can implement to enhance their overall quality of life.
One of the cornerstones of lifestyle interventions for depression is physical activity. Numerous studies have shown that regular exercise can have profound effects on mood regulation and symptom reduction in individuals with depression. Aerobic exercises such as walking, jogging, swimming, or cycling have been particularly effective in boosting endorphin levels, improving sleep quality, and reducing feelings of anxiety and stress. Engaging in strength training exercises can also promote feelings of empowerment and self-efficacy, which are often compromised in individuals with depression. Incorporating physical activity into one’s daily routine not only enhances physical health but also serves as a powerful tool for managing depressive symptoms.
- Nutrition plays a significant role in mental health and can influence the onset and severity of depressive symptoms. Research suggests that certain dietary patterns, such as the Mediterranean diet, rich in fruits, vegetables, whole grains, lean proteins, and healthy fats, may be associated with a lower risk of depression. Foods rich in omega-3 fatty acids, such as fatty fish, flaxseeds, and walnuts, have been shown to have mood-stabilizing effects and may help reduce inflammation in the brain. Conversely, a diet high in processed foods, refined sugars, and unhealthy fats has been linked to increased inflammation and oxidative stress, which can exacerbate depressive symptoms. By adopting a balanced and nutritious diet, individuals can nourish their bodies and minds, supporting overall mental well-being.
- Sleep hygiene is another critical aspect of lifestyle interventions for managing depression. Sleep disturbances are common symptoms of depression, and poor sleep quality can exacerbate mood instability and cognitive dysfunction. Establishing a consistent sleep schedule, creating a relaxing bedtime routine, and practicing good sleep hygiene habits can improve sleep quality and enhance mood regulation. Limiting caffeine and alcohol consumption, avoiding screens before bedtime, and creating a comfortable sleep environment can promote restorative sleep and contribute to better mental health outcomes.
- Stress management techniques are essential for individuals with depression to cope with the challenges of daily life. Chronic stress can exacerbate depressive symptoms and contribute to feelings of overwhelm and burnout. Mindfulness practices such as meditation, deep breathing exercises, and progressive muscle relaxation can help individuals cultivate present-moment awareness and develop resilience in the face of stressors. Engaging in hobbies, creative activities, or spending time in nature can serve as outlets for self-expression and emotional release, providing a sense of purpose and fulfillment. By incorporating stress-reduction techniques into their daily routines, individuals can build emotional resilience and enhance their ability to cope with depression.
The Impact of Depression on Cognitive Functioning
Depression can significantly impact cognitive functioning in various ways, affecting memory, attention, executive function, and processing speed. Here’s a breakdown of some key impacts:
- Memory: Depression can impair both short-term and long-term memory. Individuals may struggle to remember recent events or details, as well as experience difficulties recalling past memories.
- Attention: Depressed individuals often have difficulties sustaining attention and may be easily distracted. This can affect their ability to focus on tasks, leading to decreased productivity and performance.
- Executive Function: Executive functions involve higher-level cognitive processes such as planning, decision-making, problem-solving, and self-control. Depression can impair these functions, making it challenging for individuals to set goals, prioritize tasks, and regulate their emotions effectively.
- Processing Speed: Depression can slow down cognitive processing speed, making tasks that require quick thinking and response more difficult. This can manifest in slower reaction times and delays in information processing.
- Verbal and Visuospatial Abilities: Some research suggests that depression can impact verbal fluency and visuospatial abilities, such as spatial perception and navigation skills.
- Learning and Problem-Solving: Depressive symptoms may interfere with learning new information and adapting to new situations. Individuals may find it harder to absorb and retain new knowledge, as well as devise effective solutions to problems.
- Rumination and Cognitive Biases: Depressed individuals often engage in rumination, repeatedly focusing on negative thoughts and feelings. This cognitive pattern can exacerbate depressive symptoms and impair cognitive functioning by consuming mental resources and reinforcing negative biases in thinking.
It’s important to note that the severity of cognitive impairment can vary among individuals and may fluctuate over time. Additionally, factors such as age, comorbid medical conditions, medication side effects, and duration of depression can influence the extent of cognitive deficits experienced.
Future Directions in Depression Research
Future directions in depression research are likely to explore a wide range of avenues aimed at improving our understanding of the disorder, refining diagnostic criteria, developing more effective treatments, and identifying preventive measures. Here are some potential areas of focus:
- Biological Markers and Mechanisms: Continued efforts to identify biomarkers associated with depression could lead to more accurate diagnosis and personalized treatment approaches. Researchers may explore genetic, epigenetic, neurobiological, and immune system factors underlying depression to uncover novel therapeutic targets.
- Neuroimaging and Brain Circuitry: Advancements in neuroimaging techniques offer opportunities to investigate structural and functional brain alterations associated with depression. Future research may focus on elucidating specific neural circuits involved in mood regulation, stress response, and emotional processing, paving the way for targeted interventions such as neuromodulation techniques (e.g., transcranial magnetic stimulation, deep brain stimulation).
- Psychosocial and Environmental Factors: There’s growing recognition of the role of psychosocial and environmental factors in depression risk and resilience. Research in this area may explore how factors such as childhood trauma, social support, socioeconomic status, and lifestyle habits interact with genetic predispositions to influence depression onset, severity, and treatment outcomes.
- Digital Health and Telemedicine: The integration of digital health technologies, including mobile apps, wearable devices, and telemedicine platforms, holds promise for enhancing access to mental health care and monitoring depression symptoms remotely. Future research may evaluate the effectiveness of digital interventions for depression management, as well as their potential to augment traditional treatments and facilitate early intervention.
- Translational and Cross-Disciplinary Approaches: Collaborative efforts between basic science, clinical research, and public health disciplines can accelerate the translation of preclinical findings into clinical practice. Multidisciplinary approaches that combine genetics, neuroscience, psychology, and epidemiology may yield comprehensive insights into depression etiology, progression, and treatment response.
How to help someone dealing with depression
Supporting someone dealing with depression requires empathy, patience, and understanding. Here are some ways you can help:
- Educate Yourself: Learn about depression to better understand what your loved one is going through. This can help you provide more effective support and avoid misconceptions about the disorder.
- Listen Without Judgment: Encourage open communication and be a supportive listener. Let your loved one express their feelings without trying to offer immediate solutions or judgment.
- Offer Practical Support: Help with everyday tasks that may feel overwhelming for someone with depression, such as cooking, cleaning, or running errands. Offer to accompany them to appointments or therapy sessions if they’re comfortable with it.
- Be Patient and Empathetic: Understand that recovery from depression takes time, and your loved one may have good days and bad days. Be patient, supportive, and validate their feelings without minimizing them.
- Encourage Treatment: Encourage your loved one to seek professional help from a therapist, counselor, or psychiatrist. Offer to help them find a suitable provider or accompany them to appointments if needed.
- Promote Self-Care: Encourage healthy habits such as regular exercise, balanced nutrition, adequate sleep, and relaxation techniques. Offer to participate in activities together that they enjoy or find relaxing.
Conclusion
In conclusion, overcoming depression is no easy feat, but it is definitely possible with the right support and resources. Taking care of your mental health is crucial, whether it’s through therapy, medication, or simply reaching out to a friend for help. It’s important to remember that everyone’s journey with depression is unique, so finding what works best for you may take some trial and error.






























Leave a Reply