
Pain management refers to a medical approach that aims to alleviate or control pain. It involves a comprehensive and multidisciplinary approach to address pain, which can be acute or chronic. The goal of pain management is not always complete elimination of pain but rather improving a person’s quality of life by minimizing pain and enhancing functionality.
Key components of pain management may include:
- Medications: Analgesic medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, muscle relaxants, and antidepressants, may be prescribed to manage pain.
- Physical therapy: Exercise, stretching, and other physical therapy techniques can help improve mobility, reduce pain, and enhance overall function.
- Interventional procedures: Minimally invasive procedures, such as injections, nerve blocks, or joint injections, may be performed to target specific sources of pain.
- Psychological support: Chronic pain can have a significant impact on mental health. Psychologists or counselors may be involved to help individuals cope with pain through techniques like cognitive-behavioral therapy (CBT).
- Alternative therapies: Complementary and alternative approaches, such as acupuncture, massage, chiropractic care, or herbal remedies, may be considered to supplement conventional treatments.
- Lifestyle modifications: Encouraging healthy lifestyle changes, such as maintaining a balanced diet, regular exercise, and stress management, can contribute to pain relief.
- Patient education: Informing patients about their condition, treatment options, and self-management strategies is a crucial aspect of pain management. This helps empower individuals to actively participate in their care.
What are the different types of pain?
Pain can be classified into various types based on different criteria, such as the duration, origin, and characteristics of the pain. Here are some common classifications of pain:
- Duration:
- Acute pain: Sudden onset and typically of short duration. It often serves as a warning signal of injury or disease and is usually responsive to treatment.
- Chronic pain: Persists over an extended period, often beyond the expected time for healing. Chronic pain can be challenging to treat and may have a significant impact on a person’s daily life.
- Origin or Source:
- Nociceptive pain: Arises from damage or inflammation to tissues and is often described as a throbbing, aching, or sharp pain. Examples include cuts, burns, or fractures.
- Neuropathic pain: Results from damage or dysfunction of the nervous system. It may feel like a burning, tingling, or shooting pain. Conditions such as diabetic neuropathy or sciatica involve neuropathic pain.
- Psychogenic pain: Pain that is not due to direct physical injury or damage but is influenced by psychological factors, such as stress or anxiety.
- Location:
- Somatic pain: Arises from the skin, muscles, or joints. It is often well-localized and can be described as sharp or dull.
- Visceral pain: Originates from internal organs and may be perceived as a deep, squeezing, or cramping sensation. Visceral pain can be challenging to localize accurately.
- Pain Pattern:
- Referred pain: Pain felt in an area away from the actual site of injury or pathology. An example is pain in the left arm during a heart attack.
- Severity:
- Mild, moderate, or severe pain: Pain intensity can vary, and healthcare providers often use scales to assess and quantify the level of pain reported by individuals.
- Purpose:
- Protective pain: Acute pain that warns of potential harm or injury, prompting the individual to take protective actions.
- Non-protective pain: Chronic pain that may persist long after the initial injury has healed and may not serve a protective function.
What are the goals of pain management?
The goals of pain management are focused on improving the quality of life for individuals experiencing pain, whether it is acute or chronic. These goals may vary depending on the nature of the pain, its underlying causes, and the individual’s overall health. Here are some common objectives of pain management:
- Reduce Pain Intensity: The primary goal is often to decrease the severity of pain to a level that is manageable and allows individuals to perform daily activities with minimal discomfort.
- Improve Functionality: Enhance the ability to engage in daily tasks, work, and recreational activities by addressing pain-related limitations and improving overall physical function.
- Promote Independence: Help individuals regain or maintain independence by managing pain in a way that minimizes the impact on their ability to perform essential activities of daily living.
- Enhance Quality of Life: Alleviate pain to improve overall well-being and quality of life. This involves addressing not only the physical aspects of pain but also its psychological and social impact.
- Minimize Medication Side Effects: If medications are part of the pain management plan, the goal is to use them judiciously to provide relief while minimizing potential side effects or complications.
- Prevent or Manage Complications: Address and prevent potential complications associated with chronic pain, such as depression, anxiety, sleep disturbances, and reduced mobility.
- Promote Self-Management: Empower individuals to actively participate in their pain management by providing education, tools, and strategies for self-care. This may include lifestyle modifications, exercise, and stress management techniques.
- Enhance Emotional Well-being: Recognize and address the emotional and psychological impact of pain, promoting mental health and coping mechanisms to reduce the emotional burden associated with chronic pain.
- Identify and Treat Underlying Causes: Determine and address the root causes of pain, whether they are related to injuries, medical conditions, or other factors, to provide more targeted and effective treatment.
- Provide Multidisciplinary Care: Utilize a team-based approach involving healthcare professionals from various disciplines, such as physicians, physical therapists, psychologists, and others, to address the diverse aspects of pain and its impact on an individual’s life.
What are the common causes of pain?
- Injury or Trauma:
- Musculoskeletal injuries: Sprains, strains, fractures, and other injuries affecting muscles, bones, ligaments, or tendons.
- Soft tissue injuries: Damage to soft tissues, such as bruises, contusions, or cuts.
- Medical Conditions:
- Arthritis: Inflammation of the joints, leading to pain and stiffness. Osteoarthritis and rheumatoid arthritis are common forms.
- Neuropathy: Nerve damage or dysfunction, resulting in conditions like diabetic neuropathy or peripheral neuropathy.
- Fibromyalgia: A disorder characterized by widespread musculoskeletal pain, fatigue, and tenderness in localized areas.
- Endometriosis: A condition where tissue similar to the lining of the uterus grows outside the uterus, causing pain, especially during menstruation.
- Interstitial cystitis: Chronic inflammation of the bladder wall, leading to pelvic pain and discomfort.
- Inflammatory Conditions:
- Inflammatory bowel disease (IBD): Conditions like Crohn’s disease or ulcerative colitis can cause abdominal pain.
- Infections: Pain can result from infections in various body parts, such as urinary tract infections, dental infections, or skin infections.
What are the pharmacological options for pain management?
Pharmacological options for pain management encompass a variety of medications that can be used to alleviate pain. The choice of medication depends on the type and severity of pain, as well as individual factors such as medical history and potential side effects. Here are some common classes of pharmacological agents used in pain management:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- Examples: ibuprofen, naproxen, diclofenac.
- Mechanism of action: Reduce inflammation and alleviate pain by inhibiting enzymes involved in the production of prostaglandins.
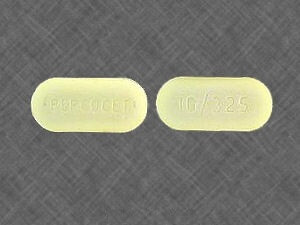
- Acetaminophen:
- Example: Tylenol.
- Mechanism of action: Reduces pain and fever but has minimal anti-inflammatory effects. It is often used for mild to moderate pain.
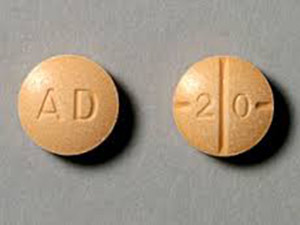
- Opioid Analgesics:
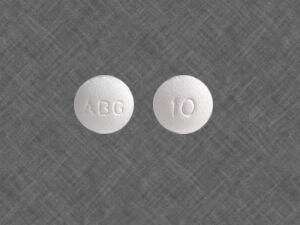
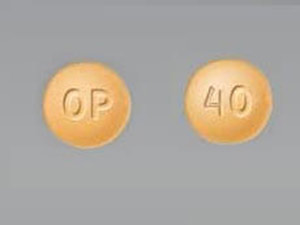
- Examples: morphine, oxycodone, hydrocodone, codeine.
- Mechanism of action: Act on opioid receptors to modulate pain perception. Opioids are often reserved for moderate to severe pain and are prescribed cautiously due to the risk of dependence and side effects.
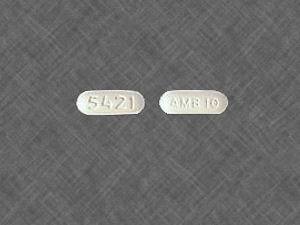
- Muscle Relaxants:
- Examples: cyclobenzaprine, baclofen, methocarbamol.
- Mechanism of action: Relax skeletal muscles, providing relief for conditions involving muscle spasms and tension.
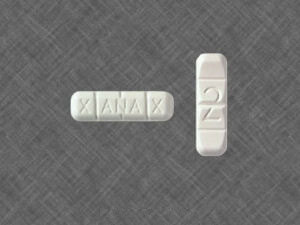
- Antidepressants:
- Examples: amitriptyline, duloxetine, venlafaxine.
- Mechanism of action: Modulate neurotransmitters in the central nervous system, providing relief for certain types of neuropathic pain.
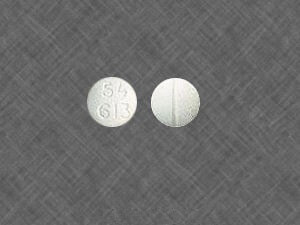
- Anticonvulsants:
- Examples: gabapentin, pregabalin.
- Mechanism of action: Stabilize abnormal electrical activity in the nervous system and are commonly used for neuropathic pain.
- Topical Analgesics:
- Examples: topical NSAIDs (e.g., diclofenac gel), lidocaine patches.
- Mechanism of action: Applied directly to the skin to provide localized relief for conditions such as osteoarthritis or postherpetic neuralgia.
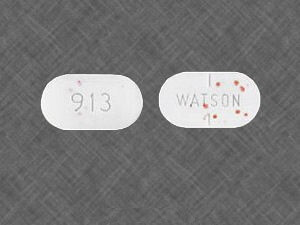
- Corticosteroids:
- Examples: prednisone, dexamethasone.
- Mechanism of action: Potent anti-inflammatory agents that can be used to reduce inflammation and pain, often administered via oral or injectable routes.
- NMDA Receptor Antagonists:
- Example: ketamine.
- Mechanism of action: Modulate the activity of N-methyl-D-aspartate (NMDA) receptors, providing relief for certain types of neuropathic pain.
How can technology be used in pain management, such as wearable devices or mobile applications?
Technology plays an increasingly significant role in pain management, offering innovative solutions to monitor, track, and alleviate pain. Here are some ways technology, including wearable devices and mobile applications, can be utilized in pain management:
- Wearable Devices:
- Biofeedback Devices: Wearable sensors can monitor physiological parameters such as heart rate variability, muscle tension, and skin conductance. By providing real-time feedback, users can learn to control their physiological responses to pain, promoting relaxation and reducing discomfort.
- Transcutaneous Electrical Nerve Stimulation (TENS) Devices: These wearable gadgets deliver low-voltage electrical currents to nerve fibers, disrupting pain signals and providing relief for various types of acute and chronic pain.
- Wearable Pain Relief Patches: These patches contain miniature devices that deliver medication or stimulate nerves to alleviate pain. They offer convenience and targeted relief for localized pain areas.
- Mobile Applications:
- Pain Trackers: Mobile apps allow users to log and track their pain levels, triggers, and medication usage over time. This data can help healthcare providers assess the effectiveness of treatment plans and make adjustments accordingly.
- Mindfulness and Meditation Apps: These apps offer guided meditation sessions, deep breathing exercises, and mindfulness practices to help individuals manage pain perception and improve overall well-being.
- Virtual Reality (VR) Therapy: VR apps immerse users in virtual environments designed to distract from pain and promote relaxation. By engaging multiple senses, VR therapy can modulate pain perception and reduce the need for pharmacological interventions.
- Telemedicine Platforms: Mobile apps facilitate remote consultations with healthcare providers, enabling patients to receive timely guidance and support for pain management strategies without the need for in-person visits.
- Data Analytics and Machine Learning:
- Advanced analytics tools can analyze large datasets generated by wearable devices and mobile apps to identify patterns, trends, and correlations related to pain management. Machine learning algorithms can personalize treatment recommendations based on individual patient characteristics, preferences, and responses to interventions.
- Education and Support:
- Mobile apps can deliver educational content, self-care tips, and coping strategies for managing pain effectively. They can also facilitate peer support networks and connect users with community resources and healthcare professionals for additional assistance.
What are the potential risks and side effects of pain medications?
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- Gastrointestinal issues: NSAIDs can cause stomach upset, ulcers, and gastrointestinal bleeding.
- Kidney problems: Prolonged use or high doses may lead to kidney damage.
- Cardiovascular risks: NSAIDs may increase the risk of heart attack and stroke, particularly in individuals with cardiovascular risk factors.
- Acetaminophen:
- Liver damage: In high doses or with excessive use, acetaminophen can cause liver damage. Individuals with liver conditions or those who consume alcohol regularly are at higher risk.
- Opioid Analgesics:
- Addiction and dependence: Opioids have a potential for addiction and dependence, especially with long-term use.
- Respiratory depression: High doses or misuse of opioids can lead to slowed breathing, which can be life-threatening.
- Constipation: Opioids commonly cause constipation and may require additional medications for management.
- Muscle Relaxants:
- Drowsiness and dizziness: Muscle relaxants can cause sedation and affect coordination.
- Antidepressants and Anticonvulsants:
- Sedation and drowsiness: These medications can cause drowsiness and affect alertness.
- Changes in mood: Antidepressants may lead to changes in mood or increased suicidal thoughts in some individuals.
What role does physical therapy play in pain management?

- Assessment and Diagnosis:
- Physical therapists assess the individual’s movement patterns, joint mobility, muscle strength, posture, and overall physical function to identify the underlying causes of pain.
- Individualized Treatment Plans:
- Based on the assessment, physical therapists develop personalized treatment plans that address the specific needs and goals of the individual. These plans may include a combination of therapeutic exercises, manual therapy, and other interventions.
- Pain Relief through Exercise:
- Therapeutic exercises are designed to improve strength, flexibility, and endurance. By targeting specific muscle groups and addressing imbalances, physical therapy can help alleviate pain and improve overall function.
- Manual Therapy:
- Hands-on techniques, such as joint mobilization and soft tissue manipulation, may be used to improve joint mobility, reduce muscle tension, and enhance overall musculoskeletal function.
- Education and Self-Management:
- Physical therapists educate individuals about their condition, contributing factors to pain, and strategies for self-management. This may include ergonomic advice, postural education, and home exercise programs.
- Modalities and Physical Agents:
- Physical therapists may use modalities such as heat, cold, ultrasound, or electrical stimulation to complement other interventions and provide pain relief.






























Leave a Reply