
Insomnia medications are pharmaceutical drugs designed to help people with insomnia, a sleep disorder characterized by difficulty falling asleep, staying asleep, or experiencing non-restorative sleep. These medications aim to improve sleep quality and duration by affecting neurotransmitters or receptors in the brain that are involved in the sleep-wake cycle. It’s important to note that while medications can be helpful in managing insomnia, they are generally considered a short-term solution, and their use should be under the guidance of a healthcare professional.
Here are some common types of medications used to treat insomnia:
- Hypnotics/Sedative-Hypnotics:
- Benzodiazepines: These drugs, such as temazepam or triazolam, act on the central nervous system to enhance the effects of the neurotransmitter gamma-aminobutyric acid (GABA), inducing sedation and promoting sleep.
- Non-Benzodiazepine Hypnotics: Drugs like zolpidem (Ambien), eszopiclone (Lunesta), and zaleplon (Sonata) also target GABA receptors but have a different chemical structure from benzodiazepines.
- Melatonin Receptor Agonists:
- Ramelteon: This medication works by interacting with melatonin receptors, which play a role in regulating the sleep-wake cycle.
- Orexin Receptor Antagonists:
- Suvorexant: This medication targets orexin receptors, which are involved in promoting wakefulness.
- Antidepressants:
- Certain antidepressants, like trazodone, amitriptyline, or doxepin, may be prescribed for their sedative effects to help with insomnia.
How do non-benzodiazepine hypnotics work?
Non-benzodiazepine hypnotics, also known as Z-drugs, work by targeting the gamma-aminobutyric acid (GABA) receptors in the brain, much like benzodiazepines. However, they do so in a more selective manner, specifically targeting the subtype of GABA-A receptors that are involved in promoting sleep. This selective action helps reduce some of the unwanted side effects associated with traditional benzodiazepines.
The three main non-benzodiazepine hypnotics are zolpidem (Ambien), zaleplon (Sonata), and eszopiclone (Lunesta). These medications are commonly prescribed for short-term treatment of insomnia. They bind to the GABA-A receptors, enhancing the inhibitory effects of GABA neurotransmission, which results in sedative and hypnotic effects, promoting sleep.
Non-benzodiazepine hypnotics typically have a shorter half-life compared to benzodiazepines, which means they are effective for helping people fall asleep but less likely to cause residual sedation the next day. However, like benzodiazepines, they can still lead to dependence and tolerance if used long-term, so they are usually prescribed for short periods of time.
Can antidepressants be used for insomnia?
Yes, certain antidepressants can be used to treat insomnia, particularly when insomnia is comorbid with depression or other mood disorders. Antidepressants that have sedating effects, such as trazodone, mirtazapine, and amitriptyline, are commonly prescribed off-label to help improve sleep in individuals with insomnia.
These medications work through various mechanisms, including antagonism of histamine receptors (which promotes drowsiness), inhibition of serotonin and norepinephrine reuptake, and modulation of other neurotransmitter systems involved in sleep regulation.
It’s important to note that while antidepressants can be effective for improving sleep, they are typically reserved for cases where insomnia is associated with depression or other psychiatric conditions. They may not be the first-line treatment for primary insomnia (insomnia not associated with another medical or psychiatric condition), and their use should be carefully monitored by a healthcare professional due to potential side effects and interactions with other medications.
What are potential side effects of hypnotic medications?
Hypnotic medications, including benzodiazepines and non-benzodiazepine drugs like zolpidem (Ambien), zaleplon (Sonata), and eszopiclone (Lunesta), can have various side effects. Common side effects include:
- Daytime drowsiness: Hypnotic medications can lead to residual drowsiness the next day, impairing cognitive function and increasing the risk of accidents.
- Dizziness and lightheadedness: These medications can cause feelings of dizziness or lightheadedness, particularly when getting up from a lying or sitting position.
- Cognitive impairment: Some individuals may experience difficulties with memory, concentration, and coordination while taking hypnotic medications.
- Tolerance and dependence: Long-term use of hypnotic medications can lead to tolerance, meaning higher doses are needed to achieve the same effect. Additionally, dependence and withdrawal symptoms can occur upon discontinuation of the medication.
- Parasomnias: These are unusual behaviors or experiences that occur during sleep, such as sleepwalking, sleep talking, or vivid dreams.
- Rebound insomnia: Abrupt discontinuation of hypnotic medications can sometimes lead to worsening insomnia, known as rebound insomnia.
- Respiratory depression: Benzodiazepines, especially at higher doses, can suppress respiratory function, particularly in individuals with underlying respiratory conditions.
How does CBT-I complement medication treatment?
Cognitive Behavioral Therapy for Insomnia (CBT-I) complements medication treatment in several ways:
- Addresses underlying causes: CBT-I targets the root causes of insomnia, such as maladaptive thoughts and behaviors related to sleep. By addressing these underlying factors, CBT-I can help individuals develop long-term strategies for improving sleep quality, even after discontinuing medication.
- Reduces reliance on medication: CBT-I aims to reduce reliance on sleep medications by teaching individuals alternative techniques for managing insomnia, such as relaxation techniques, sleep hygiene education, and cognitive restructuring. This can lead to decreased medication use or even complete cessation of medication in some cases.
- Enhances treatment effectiveness: Combining CBT-I with medication treatment can enhance the effectiveness of both approaches. Research has shown that individuals who receive combined treatment often experience greater improvements in sleep outcomes compared to those who receive medication alone.
- Minimizes side effects: CBT-I can help minimize the side effects associated with sleep medications by reducing the need for high doses or long-term use. By learning effective sleep management strategies, individuals may experience fewer medication-related side effects and improve their overall well-being.
- Promotes long-term sustainability: Unlike medication, which typically provides temporary relief, CBT-I offers long-lasting benefits by equipping individuals with skills to manage insomnia independently. This promotes sustainability and reduces the likelihood of relapse once treatment is discontinued.
why we use Insomnia Medications?
Insomnia medications are used to help individuals with persistent sleep difficulties achieve better sleep quality and duration. They are typically prescribed when non-pharmacological interventions such as improving sleep hygiene, relaxation techniques, and cognitive behavioral therapy for insomnia (CBT-I) have not been effective or when the insomnia is severe and causing significant distress or impairment in daily functioning.

What are the different types of insomnia medications?
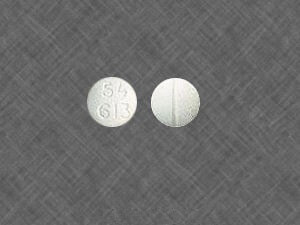
- Benzodiazepines:
- Examples: Temazepam, triazolam, estazolam.
- Mechanism: Enhance the effects of GABA, a neurotransmitter that induces sedation.
- Non-Benzodiazepine Hypnotics:
- Examples: (Ambien), eszopiclone (Lunesta), zaleplon (Sonata).
- Mechanism: Act on GABA receptors similar to benzodiazepines but have a different chemical structure.
- Melatonin Receptor Agonists:
- Example: Ramelteon.
- Mechanism: Mimics the action of melatonin, a hormone regulating the sleep-wake cycle.
- Orexin Receptor Antagonists:
- Example: Suvorexant.
- Mechanism: Blocks the action of orexin, a neurotransmitter promoting wakefulness.
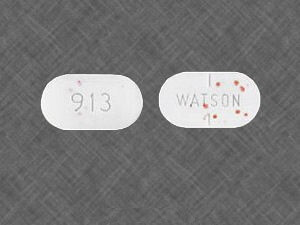
- Antidepressants:
- Examples: Trazodone, amitriptyline, doxepin.
- Mechanism: Some antidepressants with sedative properties are prescribed for insomnia.
What are the risks of long-term use of insomnia medications?
Long-term use of insomnia medications, whether they are benzodiazepines, non-benzodiazepine hypnotics, or other types, can pose several risks. It’s crucial to note that the risks can vary depending on the specific medication. Here are some general risks associated with the prolonged use of insomnia medications:
- Tolerance: Over time, the body may develop tolerance to the sedative effects of the medication, requiring higher doses to achieve the same sleep-inducing effect.
- Dependence: Long-term use of certain medications, particularly benzodiazepines, can lead to physical and psychological dependence. Abrupt discontinuation may result in withdrawal symptoms such as rebound insomnia, anxiety, and agitation.
- Cognitive Impairment: Some insomnia medications can cause cognitive side effects, including drowsiness, dizziness, and impaired concentration, which may persist with long-term use.
- Increased Fall Risk: Sedative effects of certain medications, especially in older adults, can increase the risk of falls and fractures.
- Daytime Impairment: Prolonged use may result in residual daytime sedation, affecting daily activities and cognitive function.
- Memory Issues: Some medications may contribute to memory problems and cognitive decline in the long run.
- Drug Interactions: Long-term use of insomnia medications may lead to interactions with other medications, potentially causing adverse effects.
- Health Conditions: Individuals with certain medical conditions, such as liver or kidney issues, may be more susceptible to the adverse effects of long-term medication use.
- Rebound Insomnia: Discontinuing some medications after long-term use may result in a temporary worsening of insomnia symptoms (rebound insomnia).
How quickly do insomnia medications work?
The onset of action for insomnia medications can vary depending on the specific medication and formulation. Here are general guidelines for some common types of insomnia medications:
- Benzodiazepines:
- Onset: Typically, these medications start working within 30 minutes to an hour after ingestion.
- Non-Benzodiazepine Hypnotics (Zolpidem, Eszopiclone, Zaleplon):
- Onset: Rapid onset, usually within 15-30 minutes.
- Melatonin Receptor Agonists (Ramelteon):
- Onset: Varies, but it generally takes about 30 minutes to an hour.
- Orexin Receptor Antagonists (Suvorexant):
- Onset: Generally within 30 minutes to an hour.
How can one safely stop taking insomnia medications?
Discontinuing insomnia medications should be done gradually and under the supervision of a healthcare professional to minimize the risk of withdrawal symptoms and rebound insomnia. Here are some general guidelines on how to safely stop taking insomnia medications:
- Consult Your Healthcare Provider:
- Before making any changes to your medication regimen, consult with your healthcare provider. They can provide guidance based on your individual health, the specific medication you’re taking, and your overall treatment plan.
- Gradual Tapering:
- In many cases, insomnia medications should be tapered gradually rather than stopped abruptly. This helps the body adjust to lower levels of the medication and reduces the risk of withdrawal symptoms.
- Follow Your Provider’s Recommendations:
- Your healthcare provider will provide a tapering schedule based on the specific medication you are taking. It may involve reducing the dose gradually over several weeks or months.
- Monitor for Withdrawal Symptoms:
- Be vigilant for any withdrawal symptoms, which may include increased insomnia, anxiety, irritability, or other symptoms. If you experience any adverse effects, contact your healthcare provider promptly.
- Consider Non-Pharmacological Approaches:
- Explore non-pharmacological approaches for managing insomnia, such as cognitive-behavioral therapy for insomnia (CBT-I), sleep hygiene practices, and lifestyle changes. These strategies can be valuable for long-term management.
- Maintain Healthy Sleep Habits:
- Establish and maintain good sleep hygiene habits, such as maintaining a consistent sleep schedule, creating a comfortable sleep environment, and avoiding stimulants before bedtime.
- Address Underlying Issues:
- Work with your healthcare provider to address any underlying issues contributing to insomnia, such as stress, anxiety, or lifestyle factors.
- Regular Follow-Up:
- Schedule regular follow-up appointments with your healthcare provider to assess your progress and make any necessary adjustments to your treatment plan
Are there specific insomnia medications recommended for certain populations?
The choice of insomnia medications for specific populations, such as the elderly or pregnant women, should be made with careful consideration of individual health factors, potential risks, and benefits. It’s crucial for these populations to work closely with healthcare providers to determine the most appropriate treatment. Here are some considerations for insomnia medications in specific populations:
- Elderly:
- Older adults may be more sensitive to the sedative effects of medications, increasing the risk of falls and cognitive impairment.
- Short-acting medications may be preferred to minimize the risk of residual sedation the next day.
- Non-pharmacological approaches, such as cognitive-behavioral therapy for insomnia (CBT-I), are often recommended as first-line treatments.
- Pregnant Women:
- The safety of many insomnia medications during pregnancy is not well-established, and potential risks to the developing fetus must be considered.
- Non-pharmacological approaches are generally preferred during pregnancy. CBT-I, sleep hygiene practices, and relaxation techniques may be beneficial.
- If medication is deemed necessary, healthcare providers may consider safer options with a lower risk of harm to the fetus, and the benefits should outweigh potential risks.
- Breastfeeding Women:
- Some medications can pass into breast milk, and the potential impact on the infant should be considered.
- Short-acting medications with a shorter half-life may be preferred to minimize exposure during breastfeeding.
- Consult with a healthcare provider to discuss the safety of specific medications during breastfeeding.
- Children and Adolescents:
- Insomnia medications are generally not the first line of treatment for pediatric populations.
- Non-pharmacological approaches and behavioral interventions are often recommended.
- If medication is considered, it should be under the close supervision of a pediatrician or sleep specialist.
- Individuals with Specific Health Conditions:
- Individuals with certain health conditions, such as liver or kidney impairment, may need adjustments in medication dosages or may be prescribed medications with lower metabolism requirements.
Yes, insomnia can be a symptom of an underlying health problem or a combination of factors. There are various medical, psychological, and lifestyle factors that can contribute to the development or exacerbation of insomnia. Some potential underlying causes of insomnia include:
- Medical Conditions:
- Chronic pain conditions (e.g., arthritis)
- Respiratory disorders (e.g., sleep apnea)
- Neurological disorders (e.g., Parkinson’s disease)
- Endocrine disorders (e.g., thyroid dysfunction)
- Gastrointestinal disorders (e.g., acid reflux)
- Psychiatric Disorders:
- Anxiety disorders
- Depression
- Post-traumatic stress disorder (PTSD)
- Bipolar disorder
- Other mental health conditions
- Medications:
- Certain medications may have insomnia as a side effect. Examples include some antidepressants, stimulants, and medications that affect the central nervous system.
- Lifestyle Factors:
- Irregular sleep schedule
- Poor sleep hygiene practices
- Excessive caffeine or alcohol consumption
- High-stress levels
- Shift work or irregular work hours
- Environmental Factors:
- Discomfort in the sleep environment (e.g., noise, light, temperature)
- Uncomfortable mattress or pillows
- Hormonal Changes:
- Hormonal fluctuations, such as those occurring during menopause, can contribute to sleep disturbances in some individuals.
Written by admin
Products Categories
-
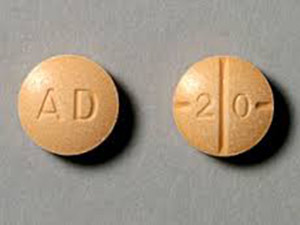 Buy Adderall Online
Buy Adderall Online -
 Buy Adipex Online
Buy Adipex Online -
 Buy Alprazolam Online
Buy Alprazolam Online -
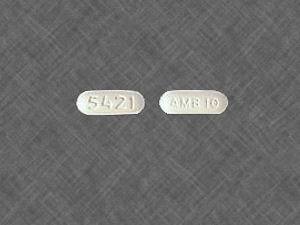 Buy Ambien Online
Buy Ambien Online -
 Buy Ativan Online
Buy Ativan Online -
 Buy Carisoprodol Online
Buy Carisoprodol Online -
 Buy Clonazepam Online
Buy Clonazepam Online -
 Buy Codeine Online
Buy Codeine Online -
 Buy Darvocet Online
Buy Darvocet Online -
 Buy Demerol Online
Buy Demerol Online -
 Buy Diazepam Online
Buy Diazepam Online -
 Buy Dilaudid Online
Buy Dilaudid Online -
 Buy Fioricet Online
Buy Fioricet Online -
 Buy Hydrocodone Online
Buy Hydrocodone Online -
 Buy Hydromorphone Online
Buy Hydromorphone Online -
 Buy Lexapro Online
Buy Lexapro Online -
 Buy Lorazepam Online
Buy Lorazepam Online -
 Buy Lorcet Online
Buy Lorcet Online -
 Buy Lortab Online
Buy Lortab Online -
 Buy Meridia Online
Buy Meridia Online -
 Buy Methadone Online
Buy Methadone Online -
 Buy Norco Online
Buy Norco Online -
 Buy Opana ER Online
Buy Opana ER Online -
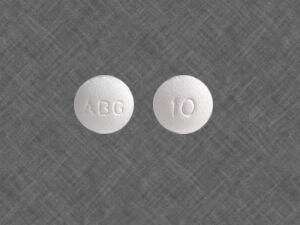 Buy Oxycodone Online
Buy Oxycodone Online -
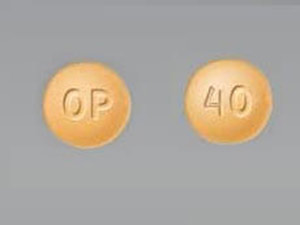 Buy Oxycontin Online
Buy Oxycontin Online -
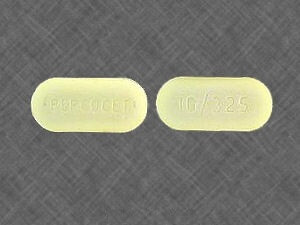 Buy Percocet Online
Buy Percocet Online -
 Buy Phentermine Online
Buy Phentermine Online -
 Buy Roxicodone Online
Buy Roxicodone Online -
 Buy Soma Online
Buy Soma Online -
 Buy Suboxone Online
Buy Suboxone Online -
 Buy Subutex Online
Buy Subutex Online -
 Buy Tramadol Online
Buy Tramadol Online -
 Buy Valium Online
Buy Valium Online -
 Buy Viagra Online
Buy Viagra Online -
 Buy Vicodin Online
Buy Vicodin Online -
 Buy Vyvanse Online
Buy Vyvanse Online -
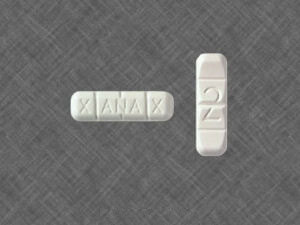 Buy Xanax Online
Buy Xanax Online

Leave a Reply